Personalised Care in Cancer
More people than ever are living with and beyond cancer. It is now widely recognised that living a good quality of life following a cancer diagnosis is as important to people as survival. Personalised Care and Support Planning (PCSP) helps people living with cancer to take an active and empowered role in the way their care is planned and delivered, with interventions and care tailored around the thing that matter most to them.
Having cancer can have an impact on every aspect of your life and on those around you. We understand that this is a difficult and often frightening time for you and your loved ones, which is why we have put together a wide range of information to help you live with and beyond cancer.
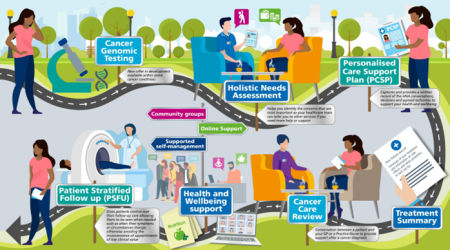
The elements of personalised care include:
- Personalised Care and Support Planning (based on holistic needs assessments) ensures people’s physical, practical, emotional, and social needs are identified and addressed at the earliest opportunity.
- End of Treatment Summaries provide both the person and their GP with valuable information, including a detailed summary of treatment completed, potential side effects, signs and symptoms of recurrence and contact details to address any concerns.
- Primary Care Cancer Care Review is a discussion between the person and their GP/primary care Nurse about their cancer journey. This helps the person to discuss any concerns, and, if appropriate, to be referred to services or signposted to information and support that is available in their community and from charities.
- Health and Wellbeing Information and Support includes the provision of accessible information about emotional support, coping with side effects, financial advice, getting back to work and making healthy lifestyle choices. This support will be available before, during and after cancer treatment.
The NHS Long Term Plan for Cancer states that: ‘After treatment, the person will move to a follow-up pathway that suits their needs and ensures they can get rapid access to clinical support where they are worried that their cancer may have recurred.’
Having supported self-management pathways means that when a person completes their primary treatment, they will be offered:
- Information about signs and symptoms to look out for, which could suggest their cancer has recurred.
- Rapid re-access to their cancer team, including telephone advice and support, if they are worried about any symptoms, including possible side-effects of treatment.
- Regular surveillance scans or tests (depending on cancer type), with quicker and easier access to results so that any anxiety is kept to a minimum.
- Personalised care and support planning and support for self-management, to help them to improve their health and wellbeing in the long-term
- Good progress has been made to implement these pathways for breast, colorectal and prostate cancers.
If you would like more information about any of the projects, please contact Macmillan Information and Support Service on 01253 955710 or Email: bfwh.



