Health inequalities are preventable, unfair and unjust differences in health between groups, populations or individuals that arise from the unequal distribution of social, environmental and economic conditions. These determine the chances of people getting ill, their ability to prevent illness, or opportunities to act and access healthcare when ill health occurs.
Fylde coast has very limited ethnic diversity but is socially and economically diverse. From affluent and elderly communities in Fylde, rural communities in Wyre and communities experiencing significant deprivation and poor health at early ages in Blackpool. Blackpool has the lowest life expectancy in England for both men and women, a result of the combination of poor-quality housing, low educational attainment and poor economic opportunities due to a predominance or seasonal employment. All these factors contribute to increased demand for healthcare whilst creating challenges for the population’s access to healthcare. BTH see this impact in the demand for our services, and we have begun to understand how socioeconomic factors impact demand and access, but there are some groups where we are unable to see healthcare inequalities – the incomplete recording of ethnicity data prevents a clear view of any healthcare inequalities faced by these minority groups, which make up less than 5% of the population.
Our Health Inequalities Steering Committee, chaired by our Medical Director, has been operational since 2023/24 and has overseen the delivery of key initiatives, including the establishment of Health Equity Champions across the Trust, who take action to tackle health inequalities in their services. During 2024/25, the Trust has delivered some key initiatives.
BTH is committed to understanding the health needs of our people, in addition to being our staff, the majority of staff also make up our local population and are therefore also our patients. A health and wellbeing questionnaire took place to help us to understand the needs of our workforce. The responses were analysed through a health equity lens as this will enable us to prioritise investment in health and wellbeing activity in areas which will have the greatest impact. The questionnaire collected data including age, gender, ethnicity, staff group, division, deprivation quintile, disability status, carer status, in addition to health behaviours and more. The staff health and wellbeing questionnaire closed on the 31st of July 2024 with a response rate of 18.3% (n=1,412).
Key findings show:
- BTH staff report worse health and wellbeing, higher rates of health harming behaviours and greater dissatisfaction with their work than national comparators.
- At least half of all staff requested the following wellbeing support: health checks, mental health and stress, healthy eating and weight management, sleep and advice on aches and pains.
- Staff with some characteristics have noticeably worse general health and experience of workplace culture: Asian and Black ethnic groups, and people with a long-term condition or disability.
- Some divisions reported a poorer experience of workplace culture a higher desire for wellbeing support.
- There was a concerning lack of confidence in managers having difficult conversations, workplace adjustments, sickness absence and return to work interviews. The results have been compared against national averages (where available).
The findings are currently being considered by senior managers and directors and plans developed to support our staff.
Health literacy is the ability of people to access, understand and use health information and services to make informed decisions to make informed decisions about their health and well-being. It’s not just about reading and understanding written information, but also about the skills, knowledge and confidence needed to navigate the health system and make effective choices. National estimates suggest that levels of health literacy are low across the Fylde Coast and the Trust recognised the need to take an organisational approach to health literacy, i.e. to make sure that we make our services and information match the needs of our population. The first stage of this work has been to deliver a health literacy programme for staff. There are now over 100 health literacy champions who have co-designed five towers of health literacy for the trust: leadership, core values, workforce, written information and verbal information. Several projects have already taken place within the trust including improving the health literature that is provided to patients to ensure they can understand what they need to do to look after their own health. Longer term evaluation will take place during 2025/26 to assess the extent to which our organisational health literacy has impacted on key metrics, such as missed appointments.
The HIV Confident Charter launched on 1st December 2024 and BTH are one of only a handful of NHS Trusts to partake and sign up to this national initiative. Blackpool Teaching Hospitals has committed to provide a stigma-free environment for all colleagues and patients who are living with HIV, by becoming a founding member of the HIV Confident charter mark.The charter mark was developed in partnership by a range of organisations including National AIDS Trust, designed to help make sure people living with HIV can work and access services with confidence.
In order to become HIV Confident, the Trust pledged to:
- Carry out a review of knowledge and attitudes across the Trust.
- Review and, where necessary, update our policies and procedures around employment, health and safety, and data protection.
- Pilot and roll-out a short anti-stigma eLearning package for all colleagues.
- Establish clear reporting processes for patients and staff who encounter stigma, so that we can address stigma where it occurs.
- Carry out a follow-up evaluation to monitor and measure the impact of this work.
The HIV programme has had great success and has resulted in an opt out service for blood borne diseases in our emergency department, which is key to identifying people and helping them into treatment. As a result of our work, we were invited to become one of the first Trusts nationally to be a HIV Confident Trust. The high pressures on the HIV service, due to the high prevalence of HIV in the population necessitates a review of arrangements to ensure it is fit for purpose in 2025/26.
The alcohol liaison team work across BTH, working and supporting patients whose alcohol use may be putting their health at risk. All patients are screened for alcohol use on admission to hospital and referred to the Alcohol Liaison Nurse Specialist team where appropriate. The team assess alcohol use, provide support and advice and where appropriate prescribe medication for alcohol withdrawal and refer to community services on discharge.
The alcohol care programme has been looking at pathways between BTH and community services. Workshops are taking place in 25/26 to develop these in more detail. This work will identify the pathway from identifying people with high alcohol consumption to treatment services. It will help partners across the Fylde Coast to understand where the links between services can be strengthened to ensure that we are providing the best service that provides people with the treatment they need to live fulfilled lives.
Vaccinations are a key public health intervention to prevent the harm caused by preventable diseases. Flu has a huge population impact and is particularly of concern for vulnerable groups such as the very young, the very old and those with long term health conditions. Nationally, flu vaccinations are provided for children aged two to three years old to help reduce their risk and reduce this group’s role in spreading infections. BTH delivered an opportunistic flu vaccination programme (October 24 to February 25) for children aged two to three years of age to support an increased rate of population coverage and help target the children who may be at highest risk of getting ill and having more severe consequences. 211 children attended clinics and of those 52 were vaccinated. These are 52 children who would not have been vaccinated. Parents found it useful to have the opportunity to have the vaccine during a clinic appointment rather than having to make an additional appointment at the GP Practice.
The NHS Equality Delivery System (EDS) is a tool designed to help NHS organisations improve services, workforce, and their leadership by focusing on equality. It involves active engagement with patients, the public, staff, and trade unions. The EDS is structured around three domains:
- Commissioned or provided services
- Workforce health and well-being
- Inclusive leadership
The EDS requires NHS organisations to use evidence and insight to evaluate and rate their performance across eleven outcomes within these three domains. This process helps ensure that trusts meet the public sector equality duty and set meaningful equality objectives. Overall responsibility for the EDS lies with trust Executive Boards.
In 2024/25, Lancashire and South Cumbria (LSC) Integrated Care Board (ICB) recommended a partnership approach to domain one for the four acute trusts in LSC, with a single service to be agreed on for the domain one ‘service case study’. Maternity services were considered the best option, due to already being part of the ‘Lancashire and South Cumbria Local Maternity System’ (LMNS) partnership.
For each domain, the evidence gathered was presented to a panel made up of the public, the Voluntary, Community, Faith and Social Enterprise (VCFSE) sector, independent evaluators and peer reviewers.
Final ratings from the NHS EDS graders is awaited, however, based on the evidence gathered and the local panel scoring, it is expected that each individual domain will be graded as ‘developing’, with the overall grade being the same.
Upon feedback from the national graders, EDS reports (incorporating local and regional actions), will be compiled for each of the three domains. These will be sent to the relevant boards and appropriate committees within the trust for comment and final agreement.
During 2025/26, the Steering Group priorities for delivery against the Health Inequalities Plan are:
- To continue to work on the health & wellbeing of our staff taking into account the findings of the survey.
- To ratify the 5 pillars of Health Literacy to be implemented across the trust
- To accelerate preventative workstreams: Delivering the HIV Prevention Programme.
- To accelerate preventative workstreams: Delivering Alcohol Care Teams.
- Data: inclusion of health equity data as part of Board of Directors performance packs; and
- Data: develop plans to improve quality data collection on all protected characteristics (for both staff and patients).
In accordance with NHS England’s statement on information on health inequalities, we will report the Blackpool Teaching Hospitals NHS Foundation Trust position in the domains relevant to our Trust:
-
Elective recovery
Indicator: Elective activity vs pre-pandemic levels for under 18s (by ethnicity and deprivation)
There has been a focus on Elective Recovery throughout the year. The Trust is part of Cohort 3 of the GIRFT Further Faster 20 programme which provides access to specialist support and additional funding to reduce elective waiting lists. This has helped with the creation of additional capacity, transformation of services and mutual aid from other providers. There was particular focus on reducing waits for under 18s and some elective activity for this cohort was moved to Saturdays to reduce the impact on education and parents taking time off work to attend with their child.
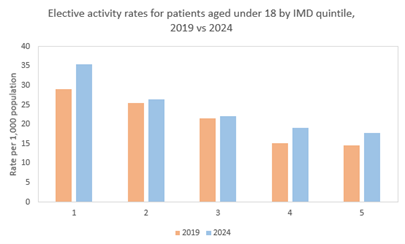
A graph of elective activity pre COVID and 2024 is presented by IMD quintile for under 18-year-olds are demonstrated in figure 1/ The graph demonstrates an increase of activity since 2019.
(note - Indices of multiple deprivation (IMD) is a measure of relative deprivation for small, fixed geographic areas of the UK. IMD classifies these areas into five quintiles based on relative disadvantage, with quintile 1 being the most deprived and quintile 5 being the least deprived).
Figure 1
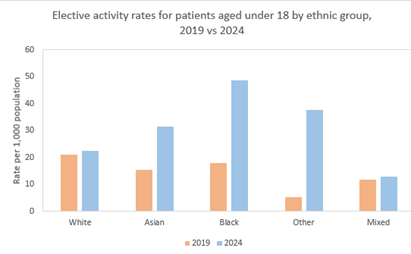
Graph of elective activity for patients under 18 by ethnicity (figure 2). (It should be noted that ethnicity data collection is a priority for us to improve, and plans are in place to address this. Data does not routinely flow from primary care for new referrals but is then a mandatory field for new registrations. Staff are encouraged to check this data with patients and an outpatient our electronic check-ins ask for this data to be validated by the patient).
Figure 2
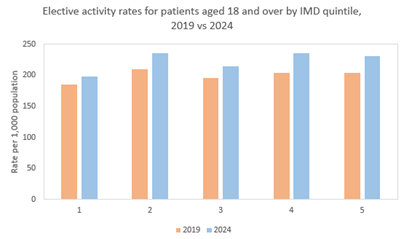
Graph of elective activity by IMD quintile pre COVID and 2024 are presented below for over 18 year olds (figure 3). The graphs demonstrate an increase of activity since 2019
Figure 3
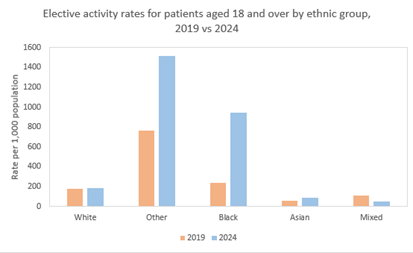
Graph by ethnicity pre COVID and 2024 is presented below for patients over 18 years of age (figure 4). (It should be noted that ethnicity data collection is a priority for us to improve, and plans are in place to address this. Data does not routinely flow from primary care for new referrals but is then a mandatory field for new registrations. Staff are encouraged to check this data with patients and an outpatient our electronic check-ins ask for this data to be validated by the patient).
Figure 4
-
Urgent and emergency care
NHS England has a plan to recover and reform urgent and emergency care services, aiming for more care in people's homes, faster ambulance response times, quicker hospital assessments, and smoother patient discharges.
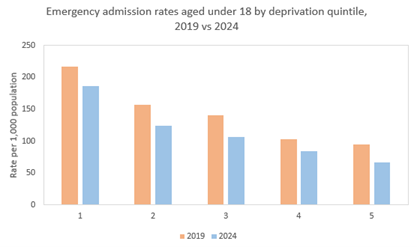
Deprivation Emergency admissions for children and young people demonstrate a clear social gradient with the rate of admissions increasing with deprivation. The admissions rate for children and young people living in our most deprived communities was significantly above the rate of those living in our least deprived communities.
Graph demonstrating urgent and emergency care activity by IMD quintile pre COVID and 2024 is presented below for under 18 year olds (figure5).
Figure 5
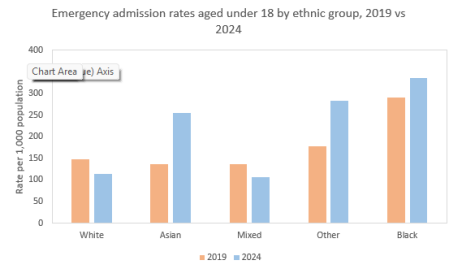
Graph by ethnicity for emergency care activity for under 18-year-olds (figure 6). (It should be noted that ethnicity data collection is a priority for us to improve, and plans are in place to address this. Data does not routinely flow from primary care for new referrals but is then a mandatory field for new registrations. Staff are encouraged to check this data with patients and an outpatient our electronic check-ins ask for this data to be validated by the patient).
Figure 6
-
Smoking cessation
Smoking is a major driver of health inequalities in England, with higher prevalence among lower-income populations. Addressing smoking cessation is crucial for reducing health disparities. As part of the Tobacco Dependency Treatment Services, the Blackpool Tobacco Addiction Service for 2024, showed the following results in 2024: -
The service achieved 496 quits, a 4.42% increase from the 2023 total of 475.
Carbon Monoxide (CO) verified quits decreased slightly in 2024 and the service achieved an average CO validation rate of 70.36%. The rate achieved was under the 85% set by the commissioners but reflects the inability of some of the clients to attend face-to-face appointments, due to poor health and the provision of some telephone support for clients working away from home.
- The service received 2,319 referrals, which was an increase of 5.12% from 2023 when there were 2,206 referrals.
- The increased number of referrals into the service fed through to a rise in the overall number of quit dates set from 981 in 2023 to 1,046 (6.63% increase). Although there have been an increase in referrals, the conversion into quits has remained high at 47.4% again up from the previous year of 44%.
- The increase in generic treatment pathway referrals which may sometimes be considered more leads than referrals may account for this change.
- There were 163 referrals from the in-house Acute Tobacco Dependence Team, and there were 86 outpatient referrals.
- As part of the Service Operational Delivery Plan, there was continuous engagement with key partners in Primary Care Networks (PCN’s) across Blackpool with the electronic referral system.
- In 2024 the service received 246 referrals from PCN’s.
- The LTFU rate on four week quit dates set decreased from 15.8% to 12.24% during the year, which may reflect the fluctuating motivation and engagement of patients accessing the service and the way in which patients are referred into service.
- Every patient who sets a quit date receives a Friends & Family Test (FFT-a customer satisfaction survey).
- In 2024, 303 clients responded to our FFT, with the level of satisfaction remaining high (good or very good) and the comments very positive. The service made efforts to increase the number of clients feeding back as the number of surveys remain low compared to the number of clients setting quit dates.
- In 2024 the service had 1046 (6.6% increase) Quit Dates set. At 12 weeks post quit date 282 of the 496 successful four week quits were still smoke free.
- Of the 282 smokefree at twelve weeks, 120 were CO validated and 162 were self-reported.
Blackpool Teaching Hospitals NHS Foundation Trust has a tobacco dependency service operating across all inpatient settings, which includes behavioural advice and provision of smoking cessation aids, including nicotine replacement therapy (NRT) and e-cigarettes. On discharge, patients are provided with a week’s supply of NRT and are referred to community smoking cessation services. Our maternity service also provides smoking cessation support, including a pilot voucher scheme to incentivise women to stop smoking whilst pregnant
-
Oral health-age 0-19
Blackpool Council commissions UCLan School of Dentistry to undertake surveys as part of the National Dental Epidemiology Programme. This is done every two years for children aged 5. Over the last 15 years the overall trend is decreasing and less than 1/3rd of children (31.1%) in Blackpool now have decay experience (National Average is 22.4%). Blackpool is ranked 26th out of 229 lower tier local authorities in England (13th out of NW LTLAs) and has similar rates to Rochdale.
Decay
- On average, the number of decayed, missing (due to decay) and filled teeth (d3mft) per child across Blackpool is 1.1 similar to the 1.05 the previous year.
- Across England the average d3mft is 0.8.
- Of the children who are experiencing dental decay, the average d3mft is 3.5 in Blackpool, the same as the England average.
Oral health indicators
- The number of decayed teeth has fallen from 3.1 to 2.7 while the number of missing or filled teeth has increased slightly. The same pattern can be seen across England
- The Care Index (filled teeth as a proportion of d3mft) shows an increase locally and nationally, increasing from 2.7% to 6.0% across Blackpool and from 7.4% to 10.5% across England.
- The Extraction Index (missing teeth as a proportion of d3mft) also shows an increase, rising from 4.3% to 13.7% across Blackpool and from 6.4% to 8.1% across England.
- Both these measures will be affected by access to dentistry and the increases seen are likely due to the continued recovery of services after the pandemic
- The proportion of children with substantial amounts of plaque has decreased from 9% to 5.4% in Blackpool while England has seen a small increase from 3% to 3.3%
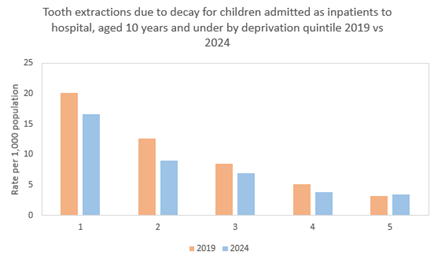
Tooth extractions
- 89% of the extractions were due to dental caries
- Blackpool had the 6th highest rate for tooth extraction with caries as primary diagnosis in England and the highest rate in the North West
- Rates in Blackpool are over three times higher than the national average, 756.4 compared to 229.2 in England
Current priorities include:
- Health Visitors distributing brushes/pastes/messages to new mums x 3 visits
- Supervised brushing (STB) in EY settings
- Fluoridated milk for all children in Years 1-6
The graph below demonstrates the rate of tooth extraction for children aged 10 and under (Figure 7).
Figure 7
The Trust’s Health Inequalities Steering Group have used the Health Inequalities Self-Assessment Tool as part of the NHS Providers package: Reducing Health Inequalities: a guide for Boards of Directors. The self-assessment includes 25 questions across four domains and provides a score and maturity rating for each in addition, the tool has suggested a series of objectives for the Trust, to develop our Health Inequalities programme. This was completed in 24/25 and will be complete the self-assessment tool at a Health Inequalities Steering Group.
The self-assessment tool was updated again 2024/25 and shown below in table 1.
1. Table - Health Inequalities self assessment results
| Theme | Maturity level |
|---|---|
| 1 - Building public health capacity and capability | Maturing |
| 2 - Data, insight, evidence and evaluation | Developing |
| 3 - Strategic leadership and accountability | Maturing |
| 4 - System partnerships | Developing |



